
What
the
medical
profession
is
seeing
today
has
not
been
witnessed
in
over
a
century.
A
viral
infection
that
is
extremely
difficult
to
treat
spread
rapidly
and
has
now
become
a
pandemic.
It
emerged
from
China
a
few
months
ago
to
cripple
the
whole
world
today.
The
last
time
such
an
endemic
occurred
was
in
1918 when the Spanish Flu killed over 25 million people.
Viruses:
Viruses
cause
a
variety
of
infection
from
a
simple
cold
to
the
deadly
Ebola
infection.
Most
of
the
serious
diseases
caused
by
them
have
now
been
conquered
through
suitable
vaccines.
However
every
now
and
again
a
new
form
evolves.
Most
of
these
are
tackled
effectively
by
the
body’s
own
immune
system.
Unfortunately
a
deadly
form
evolves
from
time
to
time
when
the
body’s
immune
system
is
unable
to
fight
it.
The
new
Corona Virus that causes “Covid 19” infection is one such. It is a respiratory virus.
How is the “New Corona Virus” different
We
have
known
about
Corona
Viruses
for
more
than
50
years.
So
why
are
we
panicking
about
this
new
virus.
By
exposure
to
many
types
of
corona
viruses
in
the
past,
our
body’s
defence
mechanism
has
acquired
suitable
antibodies
to
fight
an
invading
virus
that
is
similar
to
the
ones
that
it
has
encountered
before.
The
New
Corona
Virus
on
the
other
hand
is
completely
different
to
the
ones
that
the
body
has
been
exposed
to
before.
Therefore
it
does
not
have
a
ready
antibody
to
fight
the
newcomer.
The
immune
system
has
to
generate
a
new
antibody
to
fight
the
virus
and
that
may
take
a
few
days.
In
addition
to
that
the
binding
capacity
(fusion)
of
the
new
corona
virus
to
human
cells
appears
to
be
more
than
100
times
stronger
than
those
of
any
previously
known corona viruses.
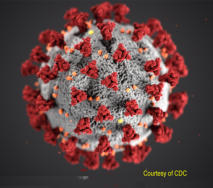
Effect of the virus when it enters the human body:
The
virus
is
so
named
because
it’s
surface
is
covered
by
bulbous
projections
that
look
like
a
crown
when
viewed
by
an
electron
microscope.
It
is
0.125
micron
in
diameter
(human
hair
is
100
microns).
The
surface
projections
are
made
up
of
protein
that
contains
the
infective
material
(the
virion).
When
an
infective
droplet
is
inhaled,
the
virus
can
reach
any
area
from
the
throat
to
the
lung
parenchyma
(the
alveolus).
For
the
virus
to
multiply
and
infect
the
individual it must first enter the living cell.
The
glycoprotein
spikes
on
the
virus
fuse
to
a
suitable
host
cell
and
inject
the
infective
material
in
to
the
cell.
An
enzyme
called
ACE2
which
is
present
on
certain
cell
membranes
like
the
lungs,
arteries,
kidneys
and
intestines
facilitates
the
spikes
to
fuse
with
the
cell.
Once
inside
the
host
cell
they
start
replicating.
The
genetic
material
of
the
virus
then
makes
the
cell
produce
several
copies
of
the
virus.
The
new
copy
can
then
enter
an
adjacent
cell
and
repeat
the process. Thus within a short time the virus starts spreading.
Symptoms
of
someone
infected
with
the
virus
may
vary
from
dry
cough,
fever
or
difficulty
in
breathing.
Some
may
even
complain
of
loss
of
taste
or
smell.
If
the
individual
is
young
and
healthy
it
may
cause
only
mild
symptoms
affecting
the
upper
respiratory
tract
giving
rise
to
fever
or
bouts
of
coughing.
However
if
they
have
other
co-existing
conditions
like
high
blood
pressure,
diabetes,
chronic
respiratory
disease,
obesity
or
if
their
immunity
is
compromised
as
when
receiving
treatment
for
cancer
etc.
the
person
may
develop
a
more
serious
form
of
the
disease
affecting
the
lung.
Older
generation
are
also
prone
to
develop
a
more serious form of the disease.
When
the
lungs
are
affected,
the
lining
membrane
of
the
alveoli
becomes
inflammed
giving
rise
to
pneumonia.
This
results
in
the
alveoli
becoming
filled
with
fluid
and
inflammatory
cells.
This
affects
the
exchange
of
gases
in
the
lung
causing
reduced
amount
of
oxygen
being
carried
in
the
blood.
When
the
disease
progresses
further,
more
of
the
lung
is
affected.
When
the
oxygen
level
in
the blood drops below a critical level all the major organs can start to fail leading to death.
Diagnostic tests for COVID 19:
(fall into two broad categories)
1
.
Swab
Test:
Molecular
tests
or
Nucleic
acid
test
of
secretions
from
the
nose
and
throat
will
detect
the
virus’
genetic
code.
2
.
Blood Test: Immunoassay will detect proteins (antigens or antibodies) associated with the virus.
Nucleic
acid-based
tests
are
the
most
sensitive
for
early
detection
of
infection.
The
test
is
called
real
time
reverse
transcription–polymerase
chain
reaction
(
real
time
RT-PCR
).
It
is
one
of
the
most
accurate
laboratory
methods
for
detecting,
tracking,
and
studying
the
corona
virus.
A
swab
from
an
individual
will
collect
mucous,
saliva,
bits
of
cells
and
with
it
viral
RNA
if
it
is
present.
The
sample
is
then
processed
in
the
lab.
Results
are
usually
available
within
a
few
hours.
Newer
machines
that
can
give you the result in under an hour are being developed and will soon be available on the market.
Covid 19 Infection