
Neonatal Jaundice
Jaundice
occurring
in
the
newborn
is
referred
to
as
neonatal
jaundice.
It
is
quite
common,
usually
harmless
and
resolves
in
two
weeks
(
physiological
jaundice
).
If
it
is
severe
and
prolonged,
it
may
be
pathological,
requiring
further
investigations
to
find the cause.
It
is
characterised
by
yellowish
discolor
ation
of
the
skin
and
eyes
due
to
accumulation
of
a
toxic
pigment
called
bilirubin
in
the
blood.
Jaundice
per
se
is
not a disease but a symptom that may signify an underlying disease.
Approximately
60% of term babies and 80% of preterm babies
develop jaundice.
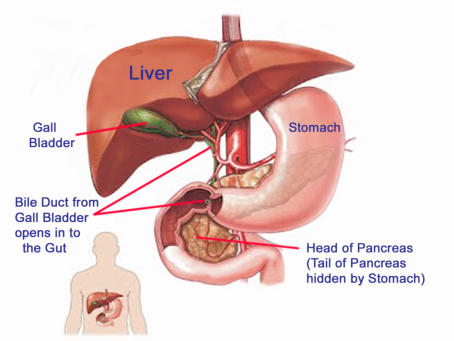
Bilirubin Formation and Excretion
One
of
the
important
sources
of
bilirubin
in
the
body
is
when
red
cells
are
broken
down
due
to
aging
of
the
cells
when
they
are
replaced
by
new
red
cells
from
the
bone
marrow.
The
bilirubin
from
red
cell
breakdown
is
processed
in
the
liver
and excreted from the body
.
Physiological Jaundice
•
The most common cause of neonatal jaundice is physiological jaundice.
•
This occurs because
newborns have more red cells than adults and hence more is broken down
.
•
Additionally the
newborn liver is immature
and unable to handle the increased amounts of bilirubin being formed.
•
This results in accumulation of bilirubin in the blood with symptoms of jaundice.
The
physiological
jaundice
described
above
usually
presents
between
day
2
–
4
after
birth,
peaks
at
one
week
and
gradually
resolves spontaneously in about two weeks
.
Pathological Jaundice
In
some
cases
however,
jaundice
is
caused
due
to
some
serious
underlying
disease
of
the
blood
or
liver.
This
is
termed pathological jaundice.
Pathological
jaundice
shows
many
of
the
following
features
•
It appears on the first day of life itself
•
Bilirubin
levels
in
the
blood
may
be
very
high
with severe jaundice
•
Baby
is
ill
and
does
not
feed
well
and
appears
irritable
•
Jaundice
is
still
present
even
after
two
weeks
(prolonged
jaundice);
the
baby
passes
pale
chalky
appearing
stools
(due
to
absence
of
bilirubin
in
the
stool)
and
dark
colored
urine
(due
to increased bilirubin pigment)
•
Enlarged
liver
and
spleen,
small
head
size
(microcephaly)
seen
in
some
congenital
infections
It
is
important
to
recognise
and
treat
pathological
jaundice
in
the
neonate
promptly
because
high
bilirubin
levels
in
the
bloodstream (hyperbilirubinemia) can result in deposition of bilurubin in the brain with serious consequences
.
Causes of Pathological Jaundice
•
ABO or Rh incompatibility between mother’s and baby’s blood group - (Increased Red cell destruction)
•
Inherited disorders of the red cell - (Increased Red cell break down)
•
Neonatal
infections
–
Toxoplasmosis,
rubella,
cytomegalovirus
(CMV),
herpes
simplex,
syphilis.
These
are
referred
to
as
TORCHS complex and should be ruled out
•
Inherited disorders of bilirubin metabolism
– Criggler Najjar syndrome, Dubin Johnson syndrome, Gilbert syndrome
•
Other uncommon causes
include diseases of the biliary system eg biliary atresia and certain inherited metabolic diseases
Jaundice in the New Born